Print This Article
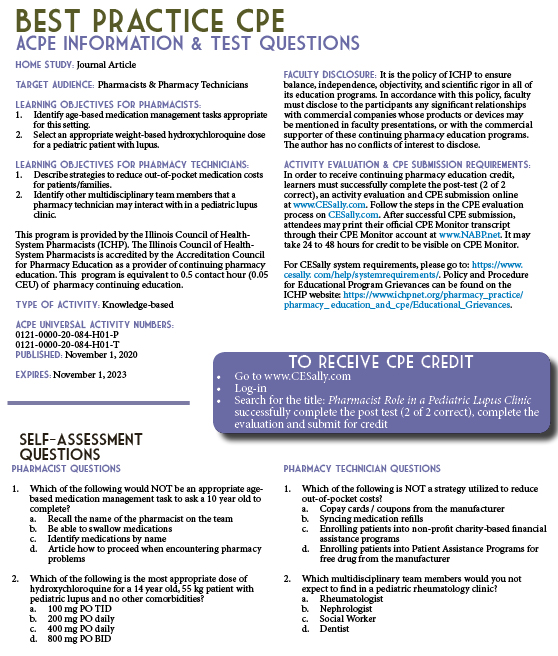
Professional Affairs - CPE Opportunity!
Pharmacist Role in a Pediatric Lupus Clinic (Best Practice Award Winner)
by Shannon M Rotolo, PharmD, BCPS, Clinical Pharmacy Specialist, UChicago Medicine, Chicago, IL; Grace Lynn Cameron, PharmD, Clinical Pharmacy Specialist, UChicago Medicine, Chicago, IL; Constantina Talevski, BA, CPhT, Ambulatory Medication Access Coordinator, UChicago Medicine Chicago, IL
Introduction, Purpose, and goals of the program
Pediatric systemic lupus erythematous (SLE) is an autoimmune disease in which the body produces pathogenic autoantibodies that cause inflammation and tissue damage.1,2 Children with pediatric SLE often require complex regimens of immunosuppressive medications to control the disease and prevent flares.3 In recent years, the incorporation of pharmacists as a part of the ambulatory care team for patients with chronic conditions, including cystic fibrosis, HIV, and others, has been described in the literature.4,5,6 The benefits vary depending on the patient population and setting, but pharmacists have been shown to improve patient and physician satisfaction, improve patients’ medication understanding and adherence, and decrease drug or vaccine related errors.7 Our institution established a Pediatric Complex Lupus Clinic in January 2019. Patients (term refers to patients, families and/or caregivers) of this clinic were scheduled to meet with a multidisciplinary care team, including a pharmacist, at their initial visit and subsequent quarterly visits. Although there is literature regarding pharmacist interactions and interventions with patients who have rheumatologic diseases, it is confined primarily to inpatient or specialty pharmacy settings, and often focused on an adult patient population.8,9,10 The purpose of this project is to describe the ambulatory pharmacist’s role in a Pediatric Complex Lupus Clinic and the impact of pharmacist involvement in clinic on patient care.
Description of the Program
Patients were scheduled for time with a pharmacist during their clinic appointments. Multiple visits were booked for the same start time, and the various care team members, including a research assistant, social worker, clinical pharmacist, advanced nurse practitioner, and attending physician rotated between rooms. When warranted, the patient’s schedule for the day might also include laboratory time for necessary blood work or an attending nephrologist. At the completion of the visits, all patients and families were encouraged to attend support groups coordinated by the Child Life Team. Two rooms were reserved: one for a patient only support group and one for a family/caregiver support group.
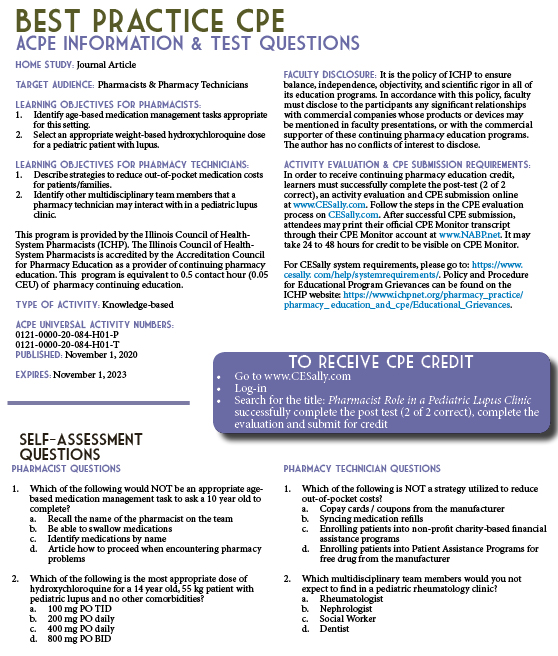
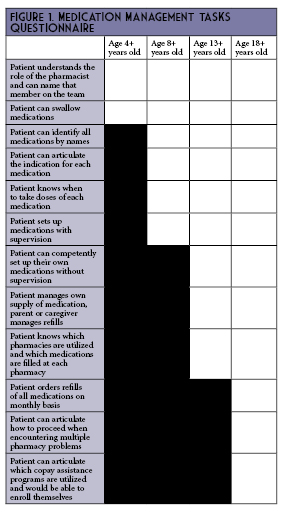
The amount of scheduled time with the pharmacist during an initial visit ranged from 20-30 minutes. This variation was due to adjustments made to the overall clinic workflow during the first several months. The actual time required to complete the initial pharmacist visit ranged from 7 to 40 minutes. Each patient was provided a pill organizer during the initial pharmacist visit. Pharmacist assessments were performed at initial and follow-up visits, and included medication reconciliation, adherence review, and medication management tasks review. Questions on the medication management tasks questionnaire (Figure 1) were age-based, and modified from a tool previously used in the Pediatric Cystic Fibrosis Clinic. Patients were given the opportunity to ask questions. If appropriate, medication management task “homework” was assigned to encourage patients to practice an additional 1-2 age-appropriate tasks prior to the time of the next visit. All patients were offered the option of transferring their prescriptions to the on-site outpatient pharmacy, which offers in-person pick-up or mail order services (e.g., refill reminder calls and free delivery). Additionally, the pharmacy team enrolled eligible patients in financial assistance programs such as manufacturer copayment savings cards, manufacturer patient assistance programs for free drug, or non-profit charity-based financial assistance programs.
The clinic was scheduled for a half-day each week, accounting for approximately 4 hours of pharmacist time. The team also conducted weekly meetings for 1 hour as a pre-huddle for the upcoming week and post-clinic discussion, in addition to using this time to touch base about on-going research, quality improvements, or other planned activities (e.g., fundraisers or patient and family events). In preparation for clinic each week, the pharmacist reviewed the patient’s chart and obtained a refill history, which accounted for an additional 1 hour of effort on average. This total time equated to a 0.15 FTE dedicated to supporting this new service line.
Experience with and Outcomes of the Program
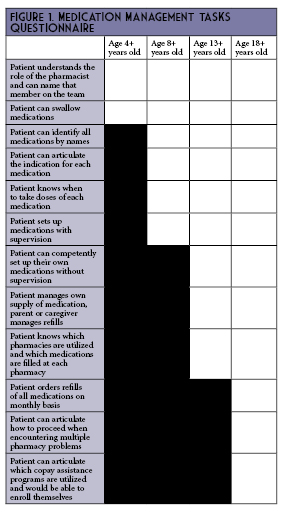
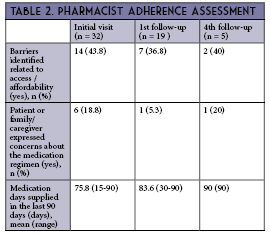
Among the 34 patients seen by a pharmacist during the 12 month study period, the median patient age was 16 years old (range 5 to 20 years old), 88.2% were female, and 47.1% were Black (Table 1). Across all visits, a barrier to medication access or affordability was identified 41% of the time (Table 2). Although the study was insufficiently powered, medication adherence did improve with subsequent pharmacist visits. At the time of the first appointment, only 67.7% of patients or parents/caregivers reported already having a relationship with a pharmacist (Table 3). The most common pharmacist education topics were review of indication for drug(s) and bone health recommendations. The most common pharmacist interventions were weight-based dose adjustment of hydroxychloroquine and de-escalation of long-standing stress ulcer prophylaxis (SUP) regimens.
Discussion of Innovative Aspects of Programs and Achievement of Goals
This is the first Pediatric Complex Lupus Clinic in the state of Illinois with a multidisciplinary model that includes a pharmacist. Our team was able to predefine the pharmacist role in this setting based on collaboration and input from other pediatric clinics at our site that already incorporate a pharmacist, such as the Cystic Fibrosis Center, and outside institutions with a Pediatric Complex Lupus Clinic supported by clinical pharmacy services, such as Nationwide Children’s Hospital in Columbus, Ohio.
A majority (75%) of questions or concerns about medication regimens were expressed to the pharmacist on the first visit, but the on-going presence of these questions through the 4th follow-up visit and persistence of barriers related to medication access /affordability reinforced our decision to have a pharmacist evaluation as a recommended component at all follow-up visits, instead of an initial pharmacist screen only.
The most common pharmacist education topics – review of indication for drug(s) and bone health recommendations – highlight the lack of prior exposure to pharmacists and dietitians for many of these patients. This is consistent with previous literature suggesting that few pediatric patients interact with community pharmacists,11 and a lack of pharmacist or dietitian involvement in the pediatric rheumatology clinic prior to the establishment of the Pediatric Complex Lupus Clinic and accompanying multidisciplinary care team. These findings were likely also influenced by the decision not to include a dietitian as part of the care team during this pilot period.
The most common pharmacist interventions – weight-based dose adjustment of hydroxychloroquine and de-escalation of long-standing SUP regimens – are also somewhat unsurprising. The American Academy of Ophthalmology updated their guidelines on the maximum recommended weight-based dose of hydroxychloroquine from 6.5 mg/kg to 5 mg/kg in 2016, based on increased risk of ocular toxicity with higher doses.12 While there was a modest decline in prescribed doses following those recommendations, higher doses remain prevalent even in 2018.13 In terms of stress ulcer prophylaxis, there is limited literature to evaluate this practice in pediatric populations outside of the pediatric intensive care unit, which likely contributes to variation in prescribing practices. Future projects for this clinic may include development of a protocol for SUP initiation and de-escalation.
Our study is limited by a small sample size and a low number of patients who completed all four quarterly visits with a pharmacist during the 12 month study period. Despite these limitations, we did see a numerically higher percentage of patients completing medication management tasks and improvements in medication adherence. Additional limitations include incomplete data on monthly prescription copayment amounts for patients who filled at outside pharmacies prior to the initial visit, all patients not completing the recommended four quarterly visits during the study timeline, and variability in the number of pharmacy staff participating in a visit due to presence of pharmacy learners rotating through this practice setting.
Conclusion
Our initial findings demonstrate that there is an opportunity for pharmacists in the outpatient Pediatric Complex Lupus Clinic setting to be involved in improving patients’ understanding of non-pharmacologic and pharmacological therapies, improving patient adherence, optimizing weight-based doses, and providing support to patients as they take on additional medication management tasks.
References
- Rahman A, Isenberg DA. Systemic Lupus Erythematosus. N Engl J Med. 2008;358:929-39.
- Tsokos GC. Systemic lupus erythematosus. N Engl J Med. 2011;365:2110-21.
- Weiss JE. Pediatric systemic lupus erythematosus: more than a positive antinuclear antibody. Pediatrics in Review. 2012;33(2):62-74.
- Young DC, et al. Patients and Families Experience With Pharmacist Care at Cystic Fibrosis Foundation Accredited Clinics. Pediatr Pulmonol. 2019 Aug;54(8):1216-1224.
- Samuel O, et al. Interdisciplinary Care Team with Pharmacist in a Community-based HIV Clinic. J Natl Med Assoc. 2018 Aug;110(4):378-383.
- Farmer EK, et al. The Pharmacist's Expanding Role in HIV Pre-Exposure Prophylaxis. AIDS Patient Care STDS. 2019 May;33(5):207-213.
- Haas-Gehres A, Sebastian S, Lamberjack K. Impact of pharmacist integration in a pediatric primary care clinic on vaccination errors: a retrospective review. J Am Pharm Assoc (2003). 2014 Jul-Aug;54(4):415-8.
- Al Hussaini M, Hammouda EI, Hammouda AE. Optimizing pharmacotherapy of systemic lupus erythematosus: the pharmacist role. Int J Clin Pharm. 2014 Aug;36(4):684-92.
- Hall JJ, Katz SJ, Cor MK. Patient Satisfaction with Pharmacist-Led Collaborative Follow-Up Care in an Ambulatory Rheumatology Clinic. Musculoskeletal Care. 2017 Sep;15(3):186-195.
- Naqvi AA, et al. Impact of pharmacist educational intervention on disease knowledge, rehabilitation and medication adherence, treatment-induced direct cost, health-related quality of life and satisfaction in patients with rheumatoid arthritis: study protocol for a randomized controlled trial. Trials. 2019 Aug 9;20(1):488.
- Abraham O, et al. Pediatric medication use experiences and patient counseling in community pharmacies: Perspectives of children and parents. J Am Pharm Assoc (2003). 2017 Jan-Feb;57(1):38-46.e2.
- Marmor MF, et al; American Academy of Ophthalmology. Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision). Ophthalmology. 2016 Jun;123(6):1386-94.
- Jorge AM, et al. Hydroxychloroquine prescription trends and predictors for excess dosing per recent ophthalmology guidelines. Arthritis Research & Therapy. 2018, 20:133.