Official Newsjournal of the Illinois Council of Health-System Pharmacists
Educational Affairs
Let's talk about it: Health Equity, Racism, and Cultural Humility
by Klodiana Myftari, PharmD, BCACP Assistant Professor of Pharmacy Practice; Midwestern University Chicago College of Pharmacy; Sally Arif, PharmD, BCPS, BCCP Associate Professor of Pharmacy Practice; Midwestern Univer
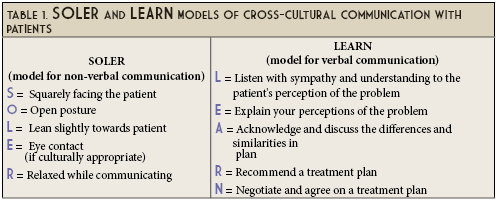
Cross-cultural communication strengthens our cultural awareness. It is a catalyst on one’s journey toward cultural humility. As individuals and healthcare providers, we move from cultural awareness to cultural knowledge when we are able to analyze the similarities and differences between our culture and that of others.8 Conversations with our patients and fellow healthcare professionals around values and beliefs that affect one’s health moves us towards cultural sensitivity. Finally, cultural competency is when we can adjust how we think and behave to support our diverse patients.8
- American Public Health Association. Health Equity. Available at https://www.apha.org/topics-and-issues/health-equity. Accessed October 6, 2020.
- Jones CP. Toward the science of practice of antiracism: launching a national campaign against Racism. Ethn Dis. 2018;28(suppl 1):231-234.
- Hook JN, Davis DE, Owen J, Worthington EL, Utsey SO. Cultural humility: measuring openness to culturally diverse clients. J Couns Psychol. 2013;60(3):353-366. [published correction appears in J Couns Psychol. 2015 Jan;62(1):iii-v].
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Devine PG, Forscher PS, Austin AJ, Cox WT. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. J Exp Soc Psychol. 2012;48(6):1267-1278.
- Berlin EA, Fowkes WC. A teaching framework for cross-cultural health care. W J Med. 1983, 139:934-938.
- Egan G. The skilled helper: a problem management and opportunity approach to helping. Pacific Grove, CA: CambridgeBrooks/Cole; 2002.
- The Winters Group, Inc. Cultural Competence ModelTM. Available at: http://www.theinclusionsolution.me/what-is-inclusion-part-2-inclusion-starts-with-i/. Accessed October 6, 2020.
- Tervalon M, Murray-García J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998;9(2):117-125.
Contents
Columns
Public Education & Awareness Outreach Publication Subcommittee
Attention ASHP Pharmacist Members
Professional Affairs - CPE Opportunity!
Features
ICHP's Newest Affiliate Leaders
Opioid Task Force - CPE Opportunity
College Connection
Midwestern University Chicago College of Pharmacy
Rosalind Franklin University College of Pharmacy
Southern Illinois University Edwardsville School of Pharmacy
University of Illinois Chicago College of Pharmacy
More
Pharmacy Action Fund Contributors
Regularly Scheduled Network Meetings
Chicago Area Pharmacy Directors Network Dinner
3rd Thursday of Odd Months
5:30pm
Regularly Scheduled Division and Committee Calls
Executive Committee
Second Tuesday of each month at 7:00 p.m.
Educational Affairs
Third Tuesday of each month at 11:00 a.m.
Government Affairs
Third Monday of each month at 5:00 p.m.
Marketing Affairs
Third Tuesday of each month at 8:00 a.m.
Organizational Affairs
Fourth Thursday of each month at 12:00 p.m.
Professional Affairs
Fourth Thursday of each month at 2:00 p.m.
New Practitioner Network
Second Thursday of each month at 5:30 p.m.
Technology Committee
Second Friday of each month at 8:00 a.m.
Chicago Area Pharmacy Directors Network Dinner
Bi-monthly in odd numbered months with dates to be determined. Invitation only.
